An Interview with the Human Immune System Regarding COVID Vaccines
As a pediatric rheumatologist, I have developed great respect for the human immune system. To me, it seems astonishingly competent and fascinatingly clever—perhaps wiser and more reliable than the human brain, at least in many ways. It is marvelous the way it has figured out how to protect us from infection. And it does this quietly and humbly, never seeking credit or reward. Yes, it occasionally makes mistakes—hence the autoimmune diseases that pediatric rheumatologists try to understand and treat—but many of those mistakes may not be its fault.
In my opinion, the most experienced, talented, and wise “expert” on immunology, virology, and vaccinology is the human immune system.
Considering how complicated the COVID-19 pandemic has become, it would seem wise to consult the human immune system to see what it would suggest, particularly regarding the development of COVID vaccines.
If our human immune system could talk, I am sure it would be happy to be interviewed, and more than happy to share its knowledge with us. Here is how I imagine that interview might go:
Pediatric Rheumatologist (PR): Thank you for taking the time to share your insights, regarding the COVID pandemic and COVID vaccines. I am sure you have been very busy, lately.
Human Immune System (HuIS): No problem. Glad to be with you.
PR: As you have probably noticed, we have scrambled to rapidly develop vaccines against the SARS-CoV-2 virus. We now have two new mRNA vaccines in use in the USA. The current goal is to vaccinate all of the world’s 7 billion people as rapidly as possible. Could you share with us how the immune system goes about developing immunity to a virus like SARS-CoV-2?
HuIS: Well, the first principle is that we (I’ll speak for my immune system teammates, because we are all on the same page and work harmoniously together) don’t like to “put all of our eggs in one basket.” By that I mean that we like to contain the virus in a variety of different ways. For example, we examine the full length of the virus to find markings on the virus that are unique to that virus and unlike any markings within our own human proteins. You see, some markings on the virus are very similar to markings on our human proteins. We would not want to produce high levels of antibodies to those markings, because they might cross-react with similar markings on our own human proteins and cause self-damage.
So, we look for the unique markings, and we produce antibodies to several of them, not to just one. That way we are not dependent on just one antibody for protection—we have multiple antibodies that work in concert.
Actually, we mobilize several other infection-fighting mechanisms (“first responders”) even before we mobilize production of the above specific antibodies. For example, we have “danger sensing” Toll receptors that quickly recognize an infectious threat and alert the entire immune system. We also use interferon, which creates an anti-viral environment, interferes with viral replication, and mobilizes other components of our immune armamentarium. We have natural killer T cells (NK cells) that kill cells that have been infected with particularly dangerous amounts of virus. And we mobilize cytokines, which accelerate and escalate the immune response. So, these “first responders” (our innate immune system) do a lot of work even before we are able to adequately mobilize our adaptive immune system (e.g., production of specific antibodies).
PR: I noticed you used the phrase “contain the virus,” rather than “kill the virus.” Why did you use those words?
HuIS: Our main goal is not necessarily to always eradicate the virus. We need viruses, and they need us. They serve a valuable purpose. They are part of our healthy microbiome. Of course, we don’t want the virus to replicate out of control and cause us to become severely ill. Viruses do not want that either, because if that happens and we die, the virus dies with us. So, the goal is to coexist peacefully with the virus. We want to allow a reasonable virus to live within us, as long as it stays under control.
We, the human immune system, are in control, though. We set the rules, and if the virus gets out of hand, we are prepared to bring it back under control, even if that sometimes requires killing it. As mentioned earlier, we achieve this control via the antibodies we produce, as well as numerous other coordinated mechanisms, which include back up mechanisms, if needed. We try hard to neither over-react nor under-react. Timing, teamwork, precision, balance, compulsive monitoring, appropriate regulation, and careful continual adjustment are needed.
Incidentally, when we choose the viral markings to which we produce antibodies, we prefer to choose markings that are least likely to provoke the virus to mutate in ways that would make the virus more lethal or more transmissible. When we produce antibodies against markings that are particularly important to the virus, like the spike protein (which allows the virus to easily enter cells), we try not to overuse that mechanism or rely only on that mechanism—because our attack on that key viral protein might provoke development of particularly worrisome mutations (that might allow for even easier entry of the virus into cells). Again, we like to employ several different control mechanisms. We want the virus to gradually become less lethal and less transmissible over time. If the virus becomes threateningly out of control, though, we are prepared to rapidly ramp up production of antibodies to key viral markings, including the spike protein (if absolutely necessary).
PR: We have developed two new COVID vaccines, based on mRNA technology. This type of vaccine has never before been used for humans. It is a vaccine that instructs cells to synthesize the spike protein of the SARS-CoV-2 virus, to which the immune system then makes anti-spike protein antibodies. There is lots of excitement and enthusiasm about this vaccine, but I am a little nervous about the safety of it, and I am not sure of its efficacy, either.
HuIS: Is that all it does—trigger the immune system to make just this one antibody, against the spike protein?
PR: Yes, do you think that is a problem?
HuIS: Well…Yes, potentially, because, for one thing, there are many tissues in the human body that have peptides that are very similar to peptides within the spike protein. We would worry that high levels of antibodies directed against the spike protein might cross-react with some of our human proteins. That could be harmful. That is why, as I said earlier, we prefer to choose antibody targets that are unique to the virus, and that is why we try to minimize production of antibodies against the spike protein (unless absolutely necessary). I can understand why the vaccine manufacturers thought to target the spike protein, because it is such an important component of the virus. But it is wiser to resist the temptation of taking that easy route, for the reasons I have already mentioned. Low levels of antibody to spike protein might be okay; but we would worry about very high levels of antibody to spike protein. We do not want to provoke the virus into mutating in a more dangerous direction. We want to encourage it to mutate in an ever less dangerous direction. Furthermore, as I have already emphasized, we like to use a multi-dimensional approach (using multiple aspects of both the innate and adaptive components of our immune system), and not rely on just a single antibody.
PR: Oh dear. I am told that the mRNA is succeeding at creating high levels of the anti-spike protein antibody, even higher than occurs with natural infection. Is that possibly not a good thing?
HuIS: Well, you don’t want to overdo things. An excessive immune reaction to a virus can cause more harm than the virus causes by itself. You need to be careful. As I have already said, we think a nuanced multi-dimensional approach is better than a one-dimensional approach. Balance, nuance, constraint, and flexibility are important.
I mention constraint and flexibility because one thing we (the human immune system) are good at is adjusting to new strains of the virus. If a new mutation is relatively benign (does not make the virus significantly more lethal or more transmissible), we leave it alone, or just slightly impair it; but if a mutation makes the virus much more threatening, we exercise our array of stronger control mechanisms. Fortunately, viruses naturally tend to mutate in ways that favor coexistence with us, rather than domination over us. Again, viruses don’t want to kill us; they want to live amicably within us. Peaceful coexistence is their goal and ours. As time goes by, a virus typically and naturally becomes increasingly more tame—to our mutual benefit. Our patient, constrained, flexible, and, yet firm control mechanisms promote this peaceful coexistence and make it more likely to occur. This is one of several reasons why once worrisome viruses have become less worrisome over time.
PR: This is all pretty complicated. Maybe we should have thought to leave all of this up to you. You clearly know what you are doing and have been doing it for a very long time. (Early modern humans evolved from an earlier hominin at least 300,000 years ago.)
HuIS: You remind me of the old Greyhound Bus commercial, “Leave the driving to us.” Perhaps you are right. Perhaps, you should leave much of this work to us, while you focus, instead, on improving the quality of peoples’ daily lives (so that they are not so susceptible to infection) and optimally treating those who develop severe COVID illness.
By the way, those patients with life-threatening COVID illness become severely ill for one or more of the following reasons: living in crowded, unhealthy, unsanitary conditions (as was enormously the case, for example, in the time of Charles Dickens); not getting healthy nutrition, exercise, rest, and sunshine; having other co-morbidities; becoming emotionally and physically stressed; not having prompt access to excellent health care; or (and this is a big reason) having an immune system that is poorly regulated (often due to subtle defects in regulatory immune response genes they were born with, and/or due to environmental toxins or manipulations that have adversely affected immune function) and, thereby, becomes excessively and dysfunctionally activated, causing a hyperinflammatory/hyperimmune state, often with cytokine storm.
So, when people become severely ill with COVID, we need you to give them superb and meticulous medical care—e.g., cleverly use corticosteroid and your anti-cytokine therapies to promptly and precisely gain control over those hyperimmune reactions. Equally important, it would be helpful if you would focus on simple preventative measures (e.g., good nutrition, healthy exercise, reduced emotional stress) and simple anti-viral treatment of early, mild SARS-CoV-2 infection—so that people would not become so severely ill in the first place. And, please, consider how environmental toxins (e.g., glyphosate) are impairing the health and function of our immune system.
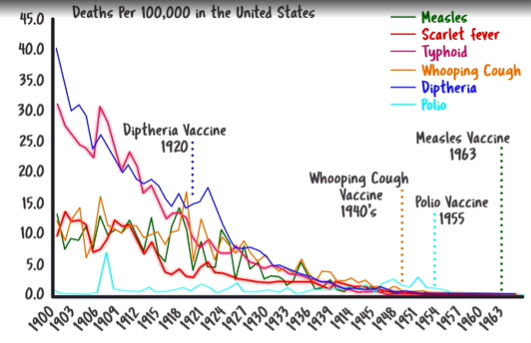
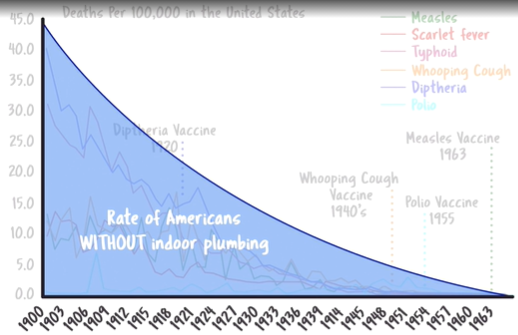
For some infectious agents there has seemed to be need for you to manufacture vaccines to help us. For example, smallpox, polio, measles, rubella, and Hemophilus influenza were difficult for us (the HuIS) to adequately manage by ourselves—at least during the 1800s, less and less so during the first half of the 20th century. In the mid-1950s and early 1960s you produced vaccines for these particularly dangerous agents. However, we hasten to point out that the most marked reduction of these worrisome infectious diseases occurred prior to the development of these vaccines. (See Graph 1.) The biggest contributor to reduction of these diseases appears to have been correction of poverty-related social conditions—over-crowding, malnutrition, poor sanitation, misery, exhaustion, physical and emotional stress, lack of sunshine, etc. (See Graph 2, which suggests that the marked reduction of many infectious diseases coincided with the marked reduction in people without indoor plumbing.) Correction of these social conditions, plus a reduction in use of environmentally toxic agents (like DDT), likely played a major role in the marked reduction of these infectious diseases that occurred even before mass vaccination was started. Many physicians, even public health officials, seem to be unaware of this correlation.
For many infectious agents it has either been unnecessary, not possible, unsafe, impractical, or otherwise unwise for you to manufacture vaccines. For example, despite great efforts, it has not been possible to manufacture successful vaccines against HIV, RSV, SARS-CoV-1, and MERS. Development of vaccines against the four most common coronaviruses has, appropriately, not been tried, despite the fact that many frail elderly people die from these ordinary coronaviruses each year. Even the vaccines against influenza viruses have been of limited value, and you should probably re-evaluate whether the vaccine approach to influenza viruses has been wise. Historically, it has been difficult to develop safe and effective vaccines against most respiratory tract viruses.
PR: So, would you say you are “Anti-Vaxx” or pro-vaccination?
HuIS: Well, that is a complex question, and I am not sure it is a helpful question. In general, thinking that is categorical, polarizing, and stereotyping is not helpful. Nuance, spectra, and levels of uncertainty need to be appreciated.
We are certainly open to the possibility that there may be certain infections for which we may need you to make vaccines—assuming that you have already adequately addressed social, cultural, and environmental issues. But we are also open to the possibility that even in those situations in which vaccination has seemed necessary (e.g., for smallpox, polio, measles, rubella, and Hemophilus influenza) a primary problem may have been environmental and social/cultural practices that made it much harder for us (the HuIS) to adequately protect the human body from severe versions of those infections. For example, it was harder for us to protect native Americans when they were given blankets laden with huge loads of smallpox virus. We probably could have handled tiny intermittent loads of smallpox, but not huge loads all at once. These days, it is harder for us to do our optimal work, if the food you eat is laden with glyphosate, or if your microbiome is otherwise imbalanced and unhealthy. Likewise, it is harder for us to protect human beings who are run down emotionally, physically, nutritionally, and spiritually. Our immune system is designed to work best when human beings are doing “all the little things” that keep their bodies, minds, and spirits healthy. Perhaps there would be less need for vaccines if environmental and cultural practices were healthier.
So, when it seems necessary to produce vaccines, is the real problem a need for the vaccine, or a need to change environmental and social/cultural practices? My HuIS teammates and I discuss this all the time. It is important to us to determine whether the need for vaccines is our fault or something that is out of our control. We do not know for sure. We are open to both possibilities.
PR: Personally, I have not been an “Anti-Vaxxer.” In fact, I was a “polio pioneer” when I was in fourth grade (in 1955) when polio appeared to be rampant. Also, during my pediatric residency (in West Virginia) I spent a huge percentage of my time treating infants and toddlers with devastating Hemophilus influenza meningitis, and I subsequently experienced how apparently protective the H flu vaccine was. So, I have been a believer in appropriate vaccinations. But until you mentioned it, I had not thought much about the possibility that there might have been environmental and social/cultural factors that made a usually achievable task almost impossible for the HuIS to accomplish—thus creating the impression that vaccination was absolutely necessary, and forever so. Come to think of it, most of those West Virginia children with H. Flu meningitis came from impoverished communities.
HuIS: Thank you for being open-minded about vaccines. Another thing my teammates and I discuss is that sometimes we get confused when our natural way of doing things is disrupted by outside manipulations. For example, it is confusing when we are suddenly bombarded by multiple vaccines all at once; and when we are repeatedly asked to react to old strains of influenza. Also, we are alarmed by many of the adjuvants the vaccine manufacturers have used to provoke a vigorous reaction on our part—as if we need to be whipped like some cowboys whip their horses. To be frank, that whipping is hurtful. Sometimes we feel micromanaged to the point of being confused as to what you want us to do. Sometimes we even lose our confidence.
PR: I appreciate what you are saying. I particularly worry about delegating the manufacture of vaccines to profiteering BigPharma corporations. I would prefer that the profit motive not be involved in vaccine production. I am glad that the polio vaccines were developed by people like Dr. Albert Sabin at Cincinnati Children’s Hospital—who was a salaried physician whose efforts did not involve interest in intellectual property rights, patents, or making money. I prefer an altruistic model for development of vaccines. I find it hard to understand why we delegate vaccine production to private, for-profit corporations, like Pfizer, who have established records of criminal activity and greed.
HuIS: We agree. We would rather work with humble, altruistic, thoughtful, honest people who see the big picture and are open-minded.
PR: The altruistic route of vaccine production is less expensive, too. I should point out to our readers, though, that the least expensive way to develop immunity is to leave that work, as much as possible, to the human immune system. You (the HuIS) have always done your work for free.
HuIS: Of course. It would never occur to us to do otherwise.
PR: Do you think the current COVID vaccines will prove to be adequately effective?
HuIS: We do not know. As mentioned earlier, it has been difficult to develop effective vaccines against respiratory tract viruses, for complex reasons. We are skeptical that the current COVID vaccines are as effective as advertised, at least in the long term. They might provide short term benefit to vaccinees; but it is conceivable that they might drive development of more worrisome vaccine-resistant strains that then threaten unvaccinated children and eventually threaten even the vaccinated. Our hope, of course, is that this conceivability will not actually happen. But this possibility certainly needs to be taken seriously.
PR: Do you think the current COVID vaccines are adequately safe?
HuIS: We don’t know. Unfortunately, the long-term safety of these vaccines has not yet been evaluated, and the jury is still out regarding short term safety. We would have recommended longer and more detailed study of safety before embarking on mass immunization. We have concerns, for the reasons mentioned earlier.
PR: Do you think COVID vaccines are necessary?
HuIS: There certainly have been many people who have died from severe COVID illness. But our guess is that most of those deaths are primarily due to excessive and dysfunctional immune reactions to the virus (not to mention social conditions and failure of the health care system at multiple levels), rather than to an extraordinarily lethal nature of the virus itself. Accordingly, it seems very important to focus on optimal treatment of those severely ill patients. To date, this has not seemed to be a top priority of the health care system.
During the early months of the pandemic, the vast majority of children and most adults under 70 appeared to be at little risk of life-threatening infection and probably did not need vaccination (if it had been available then). Children probably already had a considerable amount of cross-reactive immunity, due to the natural immunity they had developed to ordinary coronaviruses. Early in the pandemic it probably would have been wisest to carefully allow these low-risk people to become naturally infected and to become naturally immune. They would have done well, with only very rare exceptions. This natural immunity probably would be better, safer, and wiser than vaccine-induced immunity, particularly in the long run. This would have resulted in eventual natural herd immunity that would be protective of all population groups, including the elderly and frail. The elderly and frail certainly need to be carefully protected during an epidemic, and there might be a role for vaccination of the elderly and frail, if such vaccination is proven to be adequately safe and adequately effective.
But I want to emphasize a concern I mentioned a moment ago. It is possible that the combination of prolonged extensive lockdown and rapid mass vaccination (which started in December 2020) is actually transforming what was a quite manageable pandemic (during the first 9 months) into an increasingly more worrisome pandemic, because this combination could be driving the virus to desperately mutate in worrisome ways. I could be wrong about this, but we have been worrying about this possibility. Though this is only a conceivability, we urge you to take this possibility seriously.
PR: Oh dear! Are you saying that our rapid mass vaccination campaign has possibly been a mistake; and are you suggesting that we should stop that campaign?
HuIS: In my opinion, it would be very wise to at least conduct a thorough re-evaluation of how this pandemic has been handled from the very beginning—including, but not limited to, the vaccination campaign. You have many excellent medical and basic scientists, as well as social scientists and philosophers. My teammates and I would suggest that an Independent International Commission be assembled to re-evaluate the pandemic. This multi-disciplinary Commission could consist of an objective and inclusive group of virologists, immunologists, infectious disease specialists, public health specialist, vaccinologists, rheumatologists, ethicists, social scientists, social philosophers, et al (including ordinary citizens), who would apply objective critical thinking and engage in respectful healthy dialogue about all aspects of the pandemic. At the very least, I would urge this out of an abundance of caution.
PR: Thank you for all of these thoughts. I feel a little embarrassed that only now, one year into the course of the pandemic, have we thought to seek your advice.
HuIS: You are very welcome. But please understand that we do not have all the answers, either. We struggle, and we make mistakes. We are only human. But we do our best, and our intentions are always altruistic. And please do not feel badly, personally, about consulting us so late in the game. In fact, your request for an interview with us is the first such request we have ever had.
It is possible that these new vaccines will prove to be marvelously effective and adequately safe. We will hope for that. But at this time, we have questions regarding safety, efficacy, necessity, and how wise it is to be immunizing on a massive scale before adequate study has been done.
PR: Again, thank you for granting us this interview. Would you like to make any closing comments?
HuIS: Well, I prefer to view this as a mutually beneficial conversation, as opposed to an interview. Better yet, I prefer to view it as a healthy, open-minded, mutually beneficial dialogue involving careful examination of issues and a willingness to re-examine long-held assumptions and other presumptions.
In closing, I would like to say that one thing we emphasize in our work is the importance of simultaneously being both conservative and revolutionary. We honor both, because both are essential. We are constantly making new adjustments and trying new ways, while conserving what has stood the test of time. We recommend that approach to problem solving.
Thank you for thinking of us. We look forward to working together with you to make best decisions about management of this COVID pandemic.
RMR
March 19, 2021
See Graphs below:
Graph #1: This graph suggests that there was already a steady and marked decline in deaths from several infectious agents before vaccinations were developed for these diseases. Also, there has been a decline in deaths for diseases like scarlet fever and typhoid, for which we have never had vaccines.
Graph #2: This graph suggests that the decrease in deaths from infectious diseases (in the USA) has coincided with the decrease in the number of Americans without indoor plumbing—suggesting that improvements in sanitation may have played a major role.
Sources of the above graphs:
Dissolving Illusions: Disease, Vaccines, and the Forgotten History. By Suzanne Humphries, MD and Roman Bystrianyk. 2015. ISBN-13: 978-1480216891.
0 Comments